February 15, 2013
The pharmaceutical and biotechnology industries have gone through periods of blockbuster drug classes, which has often resulted in one or more leading drugs catapulting the respective company’s growth rates and, in many cases, market capital, to the very top of the industry. Examples include statins (e.g., Lipitor, Crestor, Zocor, etc.) in the classic small molecule pharmaceutical sector and anti-TNF inhibitors (Remicade, Humira, Enbrel, etc.) in the biotechnology sector. Several new classes have emerged recently that are beginning to exhibit promising, it not remarkable clinical trial results. While there is often a Best-In-Class drug in any race for biopharma gold, history shows there is often room for more than one successful product. For biotech companies in particular, the leverage of a multibillion drug is obvious.
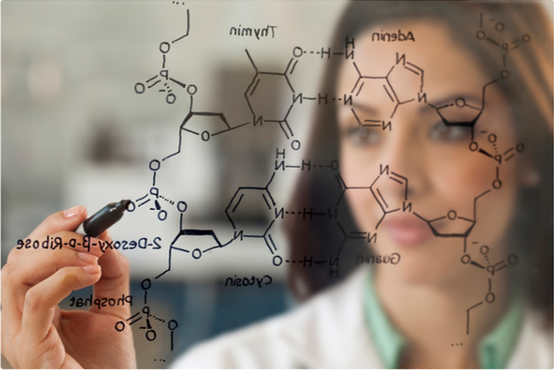
In our January 4 Issue (#745), we mentioned that “…in 2012 biotech investors witnessed the beginning of a major sea change in biopharmaceutical development…†Biotechnology/pharmaceuticals are on the verge of developing more targeted pills that have wide therapeutic windows – which are more effective and in some cases safer than the first generation biotech blockbusters. The majority of previous blockbuster drugs were enzyme inhibitors – which bind to enzymes (or proteins) and decrease their activity – and were developed by combinatorial chemistry and high-throughput screening. New technologies such as rational drug design, molecular docking and molecular mechanics use the three-dimensional structure of an enzyme’s active site to further predict affinity and specificity of novel inhibitors. The explosion in technology has led scientists to discover which “targets†make the most sense and how to design the exact compound a wider therapeutic window than ever seen before. Hence, the next generation of “super pills.â€
Investors are beginning to take note. Below we summarize five new classes of drugs being developed for broad chronic illnesses such as hepatitis, cancer, autoimmune disorders, and cardiovascular disease that, based upon a growing database of successful human clinical trials, will make up the next generation of commercial blockbusters.
HCV COMBINATIONS
The first disease benefitting from the targeted therapy revolution is the hepatitis C virus (HCV). The first company to deliver was Vertex with Incivek, a direct HCV protease inhibitor, almost $1 billion in its first full year of launch (2011). However, as a first-generation HVC inhibitor Incivek needs to be given three times a day and in combination with interferon and ribavirin – a rather cumbersome and somewhat toxic combination therapy. Nonetheless, billion-dollar status was almost instantaneous.
The HCV landscape has changed dramatically, with various studies multiple targets leading to an impressive cure rate. Enthusiasm is growing for the various interferon (IFN)-free therapies on the horizon for patients with hepatitis C virus (HCV) infection. At the recent annual meeting of the American Association for the Study of Liver Diseases (AASLD), The Liver Meeting 2012, four of the six late-breaking abstracts and a slew of other studies discussed new oral regimens that can be used to achieve high rates of sustained virologic response (SVR) in a variety of HCV patient cohorts, including null responders. The new combinations include a nucleotide/nucleoside inhibitor, a non-nuc (e.g., polymerase) inhibitor and an NS5A inhibitor. Big pharmas and big bios have spent huge amounts of money not only developing these drugs, but have acquired many of the smaller players that, as is usually the case, made many of the discoveries in the first place.
Gilead Sciences, the global antivirals powerhouse, appears to be at the top of the HCV race via their $11 billion acquisition of Pharmasset in 2011 (while VRUS was in Phase II studies). GS-7977/GS-5885, the lead combination single pill oral therapy, is in registration trials and various back-up compounds are in earlier studies. While we do not cover HCV drugs in our portfolio, Abbott Labs’ drug spinoff, AbbVie also has a strong all oral, interferon-free offering with ABT-450r/ABT-267, as is likely the best-positioned competitor to Gilead. Bristol-Myers spent $2.5 billion to acquire Inhibitex (2012) despite potential tox issues that recently doomed its first-generation compound. Nonetheless, BMS is still (a somewhat distant participant) in the field with two compounds, DMS-650032/BMS-79052. Johnson & Johnson’s TMC-435 is a protease inhibitor discovered by Tibotec (which JNJ acquired in 2002), and is in multiple trials with other HCV drugs, including interferon/ribavirin which might therefore render it obsolete before it’s approved. Merck, Boehringer Ingelheim and Achillion are also players, albeit earlier, in the HCV race.
BTK INHIBITORS
One of the hottest areas of drug research with applications in cancer and autoimmune diseases are BTK inhibitors. Bruton’s Tyrosine Kinase (BTK) is a key cell signaling enzyme that is found in blood cells, especially B-cells. B-cell activation is driven by the B-cell receptor (BCR), and BTK is a crucial part of the BCR signaling pathway. Inhibitors of BTK act downstream of the BCR and block BTK activity, and therefore, targeted inhibition of BTK is a novel approach for treating many different human diseases associated with the inappropriate activation of B-cells, including B-cell malignancies, and potentially autoimmune and inflammatory disorders. An easy-to-understand description of BTK inhibition is in the following link from the PCYC corporate website: http://www.pharmacyclics.com/btk_inhibitors_animation.html.
As a once-daily pill with unprecedented efficacy and long-term safety evidenced in studies in patients with chronic lymphocytic leukemia (CLL) small lymphocytic lymphoma (SLL), mantle cell lymphoma (MCL) and diffuse large B-cell lymphoma (DLBCL), Pharmacyclics’ ibrutinib is, by far, the leader in the BTK race. Amongst other Orphan Drug and Fast Track designations, ibrutinib recently received a Breakthrough Therapy Designation by the FDA, which will accelerate approval in MCL by next year. Johnson & Johnson invested >$1 billion in cash for ex-US rights and roughly 50% ownership of ibrutinib.
Other BTK inhibitors are under development, some by way of M&A as well. Celgene acquired Avila (in January 2012 for $350 million plus milestones), and has begun trials with AVL-292 in several similar indications as ibrutinib, and Japan’s Ono Pharmaceuticals has initiated studies with ONO-4059.
Multiple billion-dollar markets are at stake and up for grabs, when sales of the injectable blockbuster Rituxan (NHL, etc. – 2012 sales of ~$7 billion) and the oral Revlimid (MDS, myeloma – 2012 sales $3.8 billion) combined for roughly $11 billion last year.
Pi3K INHIBITORS
Another hot enzyme target that is over-activated (and in front of BTK) in the B-cell receptor pathway is Pi3K. The phosphoinositide 3-kinases (PI3Ks) are a family of enzymes involved in key immune cell functions, including cell proliferation and survival, cell differentiation and cellular trafficking. PI3K-delta and PI3K-gamma, two isoforms of PI3K, play key roles in inflammatory and autoimmune diseases. Similarly to BTK, in certain hematologic malignancies, PI3K inhibition contributes to the survival and proliferation of cancer cells and therefore, have therapeutic potential across a broad range of both inflammatory diseases and hematologic malignancies.
With multiple isoforms of the enzyme available as targets (see MOA in tables above and below), multiple compounds are being investigated in not only hematological malignancies but also in autoimmune disease. (In fact, an early ibrutinib preclinical study completely reversed arthritis in a mouse model.) PI3K is a very crowded field.
Since the BTK and Pi3K enzymes are both along the B-cell signaling cascade, a handful companies have developed inhibitors to both (i.e., dual inhibitors and BTK-Pi3K inhibitors). With another acquisition (Calistoga Pharma in 2011 for $375 million), Gilead has taken an aggressive stance to develop B-cell disorders. While the data is not in the same league as Pharmacyclics/JNJ’s ibrutinib, GS-1101 has shown impressive results and is in Phase III trials for CLL in combination with ofatumumab. An earlier-stage compound gaining momentum is Infinity’s IPI-145, which blocks the gamma and delta isoforms. Early IPI-145 data presented at ASH suggests it may be more potent than GS-1101, with a potentially cleaner side effect profile. Although earlier than the leaders in the cancer field, Infinity has explored IPI-145 in early an early pilot trial for asthma, which was favorably received at last year’s ACR meeting. Without a large partner and an active compound, Infinity may be ripe for partnership and/or acquisition.
While the market for hematological malignancies for the new classes of inhibitors is no doubt large, there does not seem to be any compound that compares with ibrutinib. Other competing drugs, such as GS-1101 and IPI-145, have promising results in a few B-cell indications, but in our view, are more likely to have a role in combination therapy and/or ibrutinib failures.
One additional class of B-cell inhibitors under development targets the Bcl-2 gene, which is implicated in similar hematologic cancers but also solid tumors, schizophrenia and autoimmunity. The lead compound in this other exciting class is AbbVie’s ABT-199, which may be used as a single agent or in combination with the BTK/PI3K inhibitors. Early data indicate that ABT-199 that might be too potent at currently investigated doses. Recently all human studies of ABT-199 were put on clinical hold ahead of planned late-stage studies, due to two patient deaths in trials from a condition known as tumor lysis syndrome. It is not clear whether the death was related to ABT-199 itself, and AbbVie (and partner Roche) are expected to resume development after the company adjusts the dosing schedule.
JAK INHIBITORS
The Janus kinase (JAK)/signal transducers and activators of transcription (STAT) signaling pathway plays an important role in cell proliferation, cell differentiation, cell migration, and cell death.
JAKs work by inhibiting the activity of one or more of the Janus kinase family of enzymes (JAK1, JAK2, JAK3, TYK2), thereby interfering with the JAK-STAT signaling pathway. It is the principal signaling mechanism for a variety of cytokines and growth factors. Over-activation of the JAK-STAT pathway leads to the release of cytokines and causing what practitioners call a “cytokine stormâ€. For example, it is the “cytokine storm†that Incyte’s Jakafi reduces which results in the relief of major symptoms, and appears to increase overall survival for MF patients. JAKs currently in development are targeting a variety of diseases, including blood cancers, RA and psoriasis.
JAKs are one of the more fruitful new classes for drug development with two drugs recently approved – INCY’s Jakafi & Pfizer’s Xeljanz. JAKs have displayed broad therapeutic activity as they are approved for both the treatment of cancer and rheumatoid arthritis (RA). JAKS are small molecules that are taken orally and have shown the ability to replace currently marketed injectable drugs, a theme we recently emphasized in “ORAL ARGUMENTS.†In addition, JAKs are small molecules (as are the rest of the “super pillsâ€) and will therefore have excellent profit margins as their manufacturing costs are a small fraction compared with COGS of a biologic.
Not unlike the PI3K enzyme, there are various forms of JAKs in development, and have different characteristics. Some selectively target one JAK and others target two or three JAKS. For example, INCY’s Jakafi targets JAK 1/2, while sparing JAK 3. Pfizer’s Xeljanz targets JAK1/3, while sparing JAK 2. INCY/LLY’s baricitinib, which is currently in Phase III trials, is very similar to Jakafi and also targets JAK 1/2. To date, Xeljanz and “bari†have both produced impressive efficacy and safety in mid- and late-stage trials, thus it appears that inhibiting different JAKs or in different ratios can lead to multiple drugs in this class. At the end of 2012, Gilead acquired YMI (for $510 million), which has CYT387 under development and is expected to start Phase III studies in 2013. Inhibiting different JAKs may eventually lead to differentiated products, as we believe there is room for multiple JAKS in autoimmune disorders, just as there are multiple blockbuster TNF inhibitors approved for RA, psoriasis and Crohn’s disease.
PCSK9 INHIBITORS
A new class of powerful cholesterol reducing drug development candidates has shown promising results in Phase II studies, potentially offering a new option for people who do not respond to drugs like Lipitor, the world’s largest selling drug with over $12 billion in annual sales before it lost patent protection in 2011. The target in this novel class is proprotein convertase subtilisin/kexin type 9, also known as PCSK9, an enzyme that in humans is encoded by the PCSK9 gene. PCSK9 regulates LDL receptors that are responsible for lowering LDL-C (bad cholesterol) in the bloodstream. Lower LDL-C is known to reduce risk of future cardiovascular complications (e.g., stroke, heart attack and death).
PCSK9 regulates the amount of LDL receptors on liver cells (hepatocytes). The greater number of LDL receptors on the liver cell, the more LDL-C is removed from the bloodstream. This lowers LDL-C levels and, in turn, risk for cardiovascular event. PCSK9 has an indirect relationship to LDL receptors: the higher the level of PCSK9, the fewer receptors are present. Hence, by inhibiting PCSK9 with an antibody, the more LDL receptors will be present on the liver cell and the more LDL-C is removed from the bloodstream.
Given the FDA’s requirement that companies run long-term outcomes trials for new cardio drugs which are targeting broad indications, staged development is the smart way to develop new drug development candidates in the PCSK9 sector. By initially targeting smaller, unmet needs, the FDA will allow the drug onto the market. Examples of this strategy are the recent approvals for both ISIS (1/13) and Agerion (12/12) in niche markets. The companies will need to perform outcomes studies down the road determining if the drugs can be used in broader cardio indications, but at least they have received regulatory approvals and are already on the market.
Regeneron/Sanofi have the most advanced PCSK9 drug candidate in development – REGN727 – which is currently undergoing a large Phase III clinical program. The Phase III ODYSSEY program includes a total of 22,000 patients. The companies are running four other Phase III studies in HeFH (n=826), statin intolerance (n=250), primary hypercholesterolemia (n=100) and high cardiovascular risk (MI, stroke, Type 2 diabetes and chronic kidney disease, n=3,716). A cardiovascular outcomes study will assess 18,000 patients who have had an acute coronary syndrome, on top of standard of care. Phase III results should start to become available in 2014, and the outcomes study will take much longer and is not slated for completion until 2018. Other companies with PCSK9 drugs under development are Amgen, Roche, Pfizer – all in Phase II studies – and an earlier-stage program at Alnylam, that recently formed a collaboration with The Medicines Company.
SELECT PCSK9 COMPOUNDS
| Compound | Company |
Status |
| REGN727 | Regeneron/Sanofi | Phase III |
| AMG145 | Amgen | Phase II |
| RG7652 | Roche | Phase II |
| RN316 | Pfizer | Phase II |
| ALN-PCS | ALNY/MDCO | Phase I |
CLASS IN SESSION
The above review is intended to summarize the hot new classes of drugs under development, and we believe that a handful of them are likely to make up the next generation of blockbuster multi-billion dollar drugs. While we only cover a few names (, INCY, CELG) and the list is by far from all inclusive, we hope readers understand what the new classes are, that there are leading drugs in each class and to be aware of the highly competitive landscape.
Next issue, we will tackle an ongoing investor debate — “Does One Buy The Class or just Best-In-Class?â€



